Response at injury site
Recovery of peripheral nerve injury is poor with only 50% of the patients regaining useful functions [Lee et al 2000]. In order to improve the cases of functional recovery through the use of medical devices, it is important to have a basic understanding of the classifications and events following a peripheral nerve injury. Peripheral injury has been classified base on the pathophysiologic features. The first being Neuropraxia or Sunderland Type I where there is local myelin damage due to compression. Axontmesis (Sunderland Type 2 to 5) is characterized by some form of loss of the continuity of axons. Neurotmesis or Sunderland Type 5 is the complete damage of the entire nerve trunk (Transection of nerve) [Lee et al 2000]. Most current treatment using devices focus on treating axontmesis and neurotmesis.
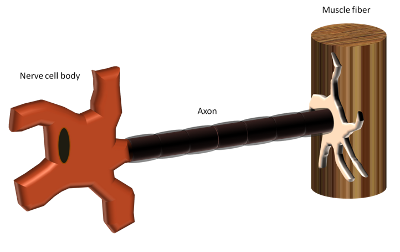
When the nerve axon is transected, Wallerian degeneration begins in about 48 h to 96 h [Lee et al 2000]. Axon distal to the gap starts to breakdown and the same applies to the myelin sheath that surrounds the distal axon. Schwann cells and macrophages begin to phagocytose the axon and myelin debris [Schmidt et al 2003]. The basal lamina distal to the injured site remains and Schwann cells align themselves to form longitudinal columns of cell bodies called Bunger bands. It is these columns that support the regenerating axons from the distal end. On the proximal end, growth cones in the form of filopodia extend towards the distal direction where the nerve axons seek out their corresponding motor end plate or sensory organs, Meissner corpuscles, Ruffini corpuscles and Merkel cells [Lee et al 2000]. If an axon does not connect with the Bunger bands in the endoneurial tubes within 3 to 4 months after the injury, progressive deposition of collagen fibers on the outer surface of the endoneurial sheath would cause the tube to collapse [Burnett et a 2004]. For gaps greater than 15 - 30 mm, the growth cones of the axon is unlikely to establish link with the distal endoneurial tube and ended up connecting to non-neural tissue, forming neuroma [Gupta S 2011].
Stage 1: Transected nerve fiber

Stage 2: Wallerian degeneration at the distal stump

Stage 3: Growth cone from proximal end

Stage 4: Connection of axon with the Bunger bands in the endoneurial tubes

Injury Classifications

| Classification
|
Pathology
|
Treatment
|
Sunderland type I
Neuropraxia
|
Local myelin damage
|
Not required
|
Sunderland type II
Axonotmesis
|
Axon loss
Endoneurium intact
Perineurium intact
Epineurium intact
|
Not required
|
Sunderland type III
Axonotmesis
|
Axon loss
Endoneurium disrupted
Perineurium intact
Epineurium intact
|
Surgery may be required to remove fibrous tissues
|
Sunderland type IV
Axonotmesis
|
Axon loss
Endoneurium disrupted
Perineurium disrupted
Epineurium intact
|
Surgery required to remove fibrous tissues
Graft required for gaps
|
Sunderland type V
Neurotmesis
|
Complete transection of nerve
|
Surgical co-aptation of nerve ends.
Graft required for gaps
|
Adapted from [Pfister et al 2011 and Lee et al 2008]
Published date: 18 April 2014
Last updated: -
▼ Reference
- Burnett M, Zager E L. Pathophysiology of Peripheral Nerve Injury: A Brief Review Neurosurg Focus 2004; 16: 5.
Open Access
- Gupta S (2011) Hand Nerve Injury Repair. Medscape 12 July 2013
Open Access
- Lee S K, Wolfe S W. Peripheral Nerve Injury and Repair. J Am Acad Orthop Surg 2000; 8: 243
Open Access
-
Pfister B J, Gordon T, Loverde J R, Kochar A S, Mackinnon S E, Cullen D K. Biomedical Engineering Strategies for Peripheral Nerve Repair: Surgical Applications, State of the Art, and Future Challenges. Critical Reviews in Biomedical Engineering 2011; 39: 81.
Open Access
▲ Close list
 ElectrospinTech
ElectrospinTech