Numerous in vitro studies have demonstrated the potential use of electrospun scaffold for bone regeneration. However, successful regeneration of bone in vivo is dependent on the requirement of the bone graft such as physical shape, mechanical requirement and graft location. Since most in vitro studies were based on electrospun two dimensional membrane, researchers have demonstrated the potential of the two dimensional membrane in calvarial defect, omentum and sterna injury which does not require thick scaffold. The electrospun membrane in this application typically functions as a guided bone regeneration graft which works as a barrier to prevent soft tissue invasion into the defect site. Several studies have shown better bone regeneration compared to the negative controls [Dimitriou et al 2012]. Current preference is to use biodegradable membrane since this negates the necessity for a second surgery to remove the membrane which may potentially disrupt the healing process. An animal study using electrospun silk fibroin membrane demonstrated a 60% new bone formation at 12 weeks which compares favorably with the 30% new bone growth in the control (no graft) specimens [Kim et al 2005].
On a 5 mm craniotomy defect was created on Sprague Dawley male rats calvarial bone, Niu et al (2017) compared the performance of electrospun membrane comprising of PLLA group, ACP-5wt%/PLLA, and HA-5wt%/PLLA group. At 8 weeks, the group with PLLA only electrospun membrane showed no bone regeneration. Only a small amount of neo-bone was formed for the HA-5wt%/PLLA group. With ACP-5wt%/PLLA electrospun membrane, the defect was fully covered by trabecular bone and the membrane fully resorbed with good integration at the defect margin. The better performance of ACP-5wt%/PLLA electrospun membrane was attributed to faster degradation and release of calcium and orthophosphate ions. Khanna et al (2017) tested the effectiveness of electrospun PCL loaded with hardystonite (HS) and PCL loaded with hydroxyapatite (HA) powders in the regeneration of 8 mm calvarial bone defect of adult Wistar male rats. HS is a calcium zinc silicate mineral and the presence of zinc and silicate has been shown in some studies to promote bone regeneration. Other controls include pure electrospun PCL scaffold and unfilled defect. In general, both PCL/HS and PCL/HA groups performed significantly better than PCL only scaffold and the group with unfilled defect. At 6 weeks the PCL/HS group showed more trabeclular bone as neo-bone at the defect interface compared to other groups. Osseointegration of the PCL/HS group was also significantly better than PCL/HA group at 12 weeks with better interfacial bonding with the surrounding bones although both PCL/HS and PCL/HA group showed no fibrous tissue infiltration between the new and old bones.
Huang et al (2021) showed the benefits of using citrate-stabilized gold-nanoparticles (GNPs) to promote osteogenesis. Coaxial electrospinning was used to form core-shell fibers with the sheath material being GNPs blended with polyvinylpyrrolidone (PVP) and ethylcellulose (EC) as the core material. Due to the water solubility nature of PVP, the GNPs can be expected to be released quickly following implantation. In a rat full thickness skull defect (5 mm) model, the group containing GNPs loaded PVP/EC scaffold showed almost complete bone coverage of the defect site after 4 weeks. In the same period, the PVP/EC group showed partial coverage with new bone and the group without any scaffolds showed a thin fibrous layer across the defect. Examination of other vital organs showed no observable tissue damage or inflammation hence demonstrating non-toxicity to metabolic and excretory organs.
Another method of encouraging and accelerating bone recovery is by the use of cell seeded scaffolds. However, conventional cell seeding on electrospun membranes only resulted in cells staying on the surface of the scaffold with little infiltration. Schuttler et al (2020) attempted to address this by simultaneously electrospinning fibers and electrospraying cells. This way, the cells would be evenly distributed throughout the scaffold. To enhance survival of the cells and reduce exposure of the cells to the toxic solvents used to prepare the polymer solution, they use culture media as a liquid fiber collector. Both PLLA (poly-l-lactide acid) and PL LA-collagen type-I nanofiber scaffolds (PLLA Col I Blend) with and without cell seeded were tested in rat full thickness critical size calvarial defects. For both PLLA electrospun scaffolds, both scaffolds with and without cells showed comparable results. However with PLLA-collagen type-I electrospun scaffolds, cell seeded scaffolds showed significantly better bone formation.
Bone morphogenic proteins (BMP) is known to significantly increase bone formation both in vitro and in vivo when incorporated with the scaffold. The positive influence of BMP-2 has also been demonstrated on electrospun scaffold. In a comparison of electrospun poly(L-lactic acid) (PLLA) scaffold with and without BMP-2 incorporated, empty defect and with bovine spongiosa graft as positive control, the electrospun scaffold with BMP-2 demonstrated significantly more new bone regeneration compared to the other study subjects at 8 weeks [Shofer et al 2011]. However, unlike other reported in vivo results, electrospun scaffold without BMP-2 does not show significant bone regeneration compared to the empty defects.
To use electrospun nanofibers membrane as a bone graft for volume defect, Kolambkar (2009) rolled the membrane to a tube form with alginate hydrogel in its lumen. The hybrid structure was then inserted into a rat femoral critical size defect. However, as the structure does not have adequate mechanical strength to support the weight of the animal, bone plates were used to stabilize the implanted area. Kolambkar used the hydrogel for controlled delivery of BMP-2 and complete filling of the defect with new bone was observed at week 12. When the electrospun membrane was perforated with holes to allow greater release of the BMP-2 to the surrounding, almost complete filling of the defect was observed at week 4. Since electrospun nanofibres scaffold alone is not mechanically stiff and strong, a hybrid structure comprising of the nanofibres and 3D printed scaffold may be more suitable for clinical application. Yun et al (2019) electrospun a poly(lactide-co-glycolide)/hydroxyapatite nanofibres sheet and roll into a thick wall cylinder with wall thickness of 2 mm. A 3D melt printing method was used to replicate the radius bone segment of the study subject, beagle dog. The 3D printed poly(lactic-acid) (PLA) scaffold has a hollow in the center which was filled in with the rolled poly(lactide-co-glycolide)/hydroxyapatite nanofibres prior to implantation into the segmental bone defect. The 3D printed PLA scaffold provided the mechanical support to maintain the shape of the assembly while the electrospun nanofibres layer is able to provide the surface topography for better cell adhesion and proliferation. During implantation, gelatine was added along with the scaffold assembly to function as glue and to promote cell adhesion. However, the scaffold assembly alone is unable to promote bone generation. Only in the group with rhBMP-2 and gelatine added during implantation showed significant bone regeneration at week 20.
Although much in vivo studies of electrospun scaffold were based on various forms of two dimensional membranes, electrospinning has also been shown to be capable of constructing three dimensional block structures.
The emergence of techniques to construct three dimensional block electrospun structures has seen some preliminary animal studies using such scaffolds. Cai et al (2012) used cross-layering of poly(L-lactic acid)/polycaprolactone nanofibrous yarn to construct a three-dimensional (3D) scaffold. Cavity defects (5 mm by 5 mm) were created in the anteroexternal area of the proximal tibia of New Zealand white rabbits and filled in with the scaffold. Mature and bony tissue was found in most part of the scaffold after week 6 and was clearly visible under the radiographs. Schneider et al (2011, 2009) used low temperature electrospinning technique where in situ ice crystals formation during electrospinning was used to build up a block fibrous structure. Perhaps due to the fact that the resultant fibrous structure is soft with cotton wool-like texture, it was used as filler in a bone cavity defect. Using a rabbit cranial defect, the amount of new bone formation after 4 weeks using poly(lactide-co-glycolide) with calcium phosphate electrospun scaffold was better but not statistically significant from using commercially available Bio-Oss [Schneider et al 2009]. In a later study using bone cavity defect at the humerus and femur of a sheep model with poly(lactide-co-glycolide) with calcium phosphate and silver calcium phosphate nanoparticles incorporated as the filler, new bone formation of about 20% was demonstrated after implantation for 2 months [Schneider et al 2011]. Unfortunately, both these studies were not able to demonstrate statistically significant better performance over the negative control (empty defect).
Mineralization has been used to strengthen the electrospun three-dimensional scaffold such that it maintains a certain level of structural integrity for implantation. Ngiam (2010) demonstrated the use of mineralized three-dimensional scaffold made out of nanofibrous yarns in a rabbit ulna defect. Instead of a cavity defect, this study was based on complete removal of a 15 mm segmental defect. Surprisingly, the percentage new bone formation for scaffold made out of poly-L-lactide/collagen and poly-L-lactide/collagen/nHA were slightly better than poly-L-lactide/collagen/nHA/BMP-2. This was attributed to the low dosage of BMP-2 used in the study. All the defects with filler scaffold showed approximately 50% new bone regeneration compared to about 38% for blank control after 3 months of implantation.
Table 1. Summary of in-vivo animal studies results of electrospun scaffolds.
|
Graft description
|
Animal model
|
Observation
|
Reference
|
|
Poly(lactide-co-glycolide)/hydroxyapatite nanofibres rolled into tube and inserted into 3D melt printed radius bone segment replica with rhBMP-2 and gelatine instilled.
|
Beagle Dog. 20 mm-long radius defect.
|
20 weeks showed noticeable new bone tissues. The mid-shaft region of the scaffold was still osteoporotic, and the host bone-scaffold junction was not fully bridged
|
Yun et al 2019
|
|
Randomly oriented silk fibroin nanofiber membrane
|
New Zealand White Rabbits. Calvarial bone defect (8 mm diameter).
|
~60% new bone growth of total defect compared with ~30% for control (no graft) at 12 weeks
|
Kim et al 2005
|
|
Randomly oriented polycaprolactone fiber membrane seeded with MSC isolated from bone marrow harvested from neonatal Lewis rats and cultured for 1 week in osteogenic medium.
|
Adult female Lewis rats. Grafted on omentum and placed in abdominal cavity
|
Mineralization occurred throughout the scaffold at 4 weeks
|
Shin et al 2004
|
|
Randomly oriented PLLA nanofiber membrane (fiber dia. 200 to 700 nm) membrane seeded with amniotic mesehchymal stem cells harvested from time-dated pregnant New Zealand does and cultured for 14.6 or 33.9 weeks in osteogenic medium in bioreactor.
|
Weaning kits (rabbit) full-thickness partial sterna resection spanning 2 to 3 intercostal spaces
|
Complete closure of defect in all animals after 2 months. No statistically significant difference for stem cells cultured for 14.6 or 33.9 weeks.
|
Steigman et al 2009
|
Fluffy, cotton wool-like PLGA/Calcium phosphate
Fluffy, cotton wool-like PLGA
Bio-Oss
|
New Zealand white rabbits, cranial circular non-critical size defects (dia 6 mm)
|
Area fractions of newly formed bone after 4 weeks
Fluffy, cotton wool-like PLGA/Calcium phosphate, 35%
Fluffy, cotton wool-like PLGA, 25%
Bio-Oss, 31%
Empty defect, 28%
|
Schneider et al 2009
|
|
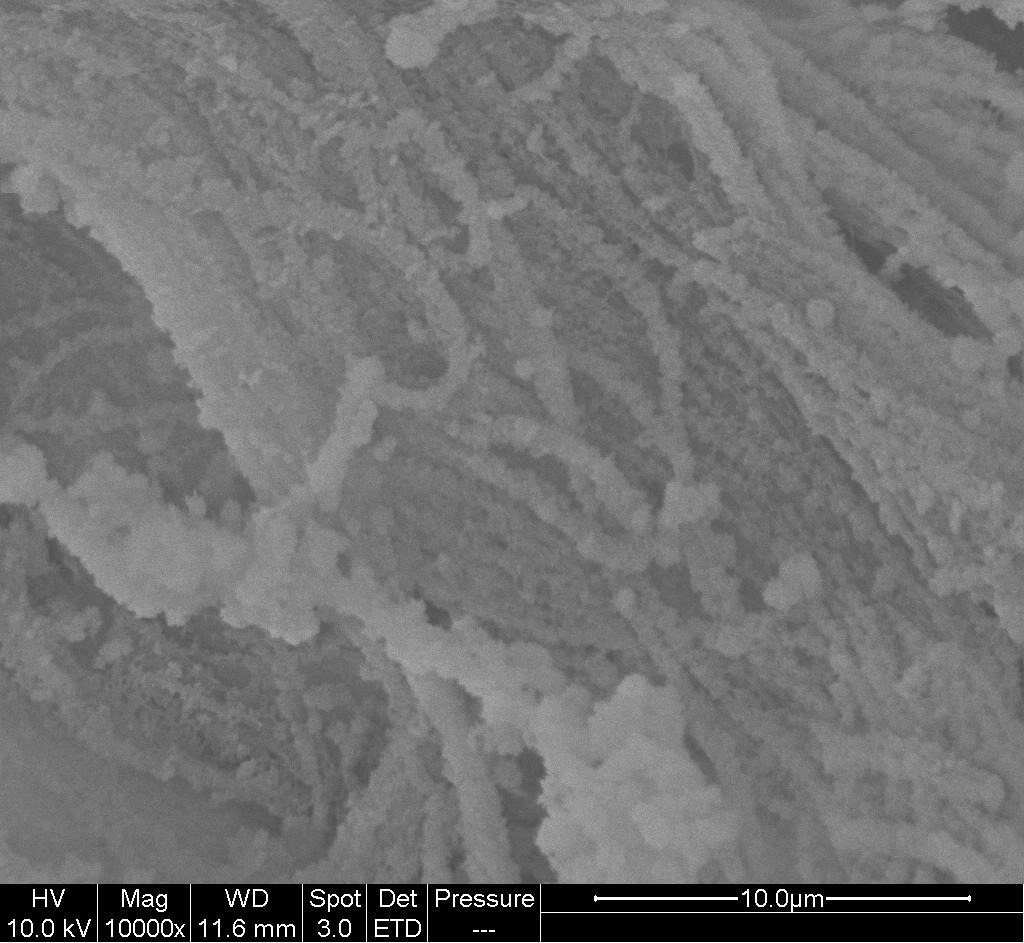
Fluffy, cotton wool-like PLGA/Calcium phosphate (fiber dia. 5 - 10 um)
|
Swiss Alpine sheep age 2.5 years and body weight 43 - 46 kg.
Hole defects (dia. 8 mm and depth 13 mm) in distal, epiphysis and proximal metaphysis of humerus and femur
|
20% new bone formation after 8 weeks.
|
Schneider et al 2011
|
|
Randomly oriented PLLA nanofiber membrane with and without BMP-2 blended.
|
Twenty five-month-old male Sprague-Dawley rats
Bilateral full thickness critical size (5 mm) calvarial defects at parietal bone.
|
New bone formation at 12 weeks
Empty cavity (negative control): 8%
Bovine spongiosa graft (positive control): 25%
PLLA scaffold: 11%
PLLA and BMP-2: 45%
|
Schofer et al 2011
|
|
Randomly oriented polycaprolactone (PCL) / poly(methyl methacrylate) (PMMA) (7:3) fiber (diameter of 2.24 um) membrane.
|
Male Sprague Dawley rats with 5 mm diameter parietal skull defect.
|
27% new bone formation after 2 months compared to 8% in negative control (empty defect)
|
Son et al 2014
|
Randomly oriented PCL membrane scaffold rolled into a tube
Randomly oriented PCL nanofibrous membrane rolled into a tube with alginate in the core
Randomly oriented PCL nanofibrous membrane rolled into a tube with alginate in the core and BMP-2 incorporated
Randomly oriented PCL nanofibrous perforated membrane rolled into a tube with alginate in the core and BMP-2 incorporated.
|
13 week old female Sasco Sprague Dawley rats femoral segmental defect (8 mm). Femora were stabilized by modular fixation plates.
|
For randomly oriented PCL nanofibrous perforated membrane rolled into a tube with alginate in the core and BMP-2 incorporated, almost completely filled with new bone at 4 weeks.
At 12 weeks, defect treated with BMP-2 loaded scaffolds were completely filled with new bones. This compared to less than 20% new bone regeneration for the other scaffolds.
|
Kolambkar 2009
|
Poly-L-lactide/collagen nanofibrous yarn three-dimensional scaffold
Poly-L-lactide/collagen/nHA nanofibrous yarn three-dimensional scaffold
Poly-L-lactide/collagen/nHA/BMP-2 nanofibrous yarn three-dimensional scaffold
|
New Zealand white rabbit, 15 mm segmental ulna defect.
|
New bone formation after 3 months,
Poly-L-lactide/collagen, 55%
Poly-L-lactide/collagen/nHA, 56%
Poly-L-lactide/collagen/nHA/BMP-2, 50%
Blank control, 38%
|
Ngiam 2010
|
In tendon/ligament injuries, one challenge is the reintegration of the ruptured tendon or ligament to the bone. Electrospun membrane has been tested positively as guided bone regeneration graft [Dimitriou et al 2012] and the same concept may be applied for re-establishment of tendon/ligament to bone interface. Chen et al (2018) tested the effectiveness of electrospun random and dual-layer aligned-random silk fbroin poly(l-lactic acid-co-e-caprolactone) (P(LLA-CL)) nanofibrous scaffolds (ARS) in tendon-to-bone healing in a rabbit extra-articular model. Autologous Achilles tendon was wrapped either in ARS or electrospun random silk fibroin/P(LLA-CL) membrane and passed through the bone tunnel, while the control group was unwrapped Achilles tendon transplanted directly. Various parameters such as ultimate load-to-failure and stiffness, collagen maturity and new bone formation was better with electrospun membrane wrap and the ARS wrap demonstrating the best results in the 12 weeks study.
Published date: 17 June 2014
Last updated: 07 February 2023
▼ Reference
-
Cai Y Z, Zhang G R, Wang L L, Jian Y Z, Ouyang H W, Zou X H. Novel biodegradable three-dimensional macroporous scaffold using aligned electrospun nanofibrous yarns for bone tissue engineering. J. Biomed Mater Res Part A 2012; 100A: 1187.
-
Cai J, Wang J, Ye K, Li D, Ai C, Sheng D, Jin W, Liu X, Zhi Y, Jiang J, Chen J, Mo X, Chen S. Dual-layer aligned-random nanofibrous scaffolds for improving gradient microstructure of tendon-to-bone healing in a rabbit extra-articular model. International Journal of Nanomedicine 2018;13: 3481
Open Access
-
Dimitriou R, Mataliotakis G I, Calori G M, Giannoudis P V. The role of barrier membranes for guided bone regeneration and restoration of large bone defects: current experimental and clinical evidence. BMC Medicine 2012; 10: 81.
Open Access
-
Huang C, Dong J, Zhang Y, Chai S, Wang X, Kang S, Yu D, Wang P, Jiang Q. Gold Nanoparticles-Loaded Polyvinylpyrrolidone/Ethylcellulose Coaxial Electrospun Nanofibers with Enhanced Osteogenic Capability for Bone Tissue Regeneration. Materials & Design 2021; 212: 110240.
Open Access
-
Khanna K, Jaiswal A, Dhumal R V, Selkar N, Chaudhari P, Soni V P, Vanage G R, Bellar J. Comparative bone regeneration study of hardystonite and hydroxyapatite as filler in critical-sized defect of rat calvaria. RSC Adv. 2017; 7: 37522.
Open Access
-
Kim K H, Jeong L, Park H N, Shin S Y, Park W H, Lee S C, Kim T I, Park Y J, Seol Y J, Lee Y M, Ku Y, Rhyu I C, Han S B, Chung C P. Biological efficacy of silk fibroin nanofiber membranes for guided bone regeneration. J Biotechnol 2005; 120: 327.
-
Kolambkar. Electrospun Nanofiber Meshes for the Functional Repair of Bone Defects. PhD Thesis. Georgia Institute of Technology 2009.
Open Access
-
Ngiam M L M. Differentiation of Bone Marrow Derived Mesenchymal Stem Cells (BM-MSCs) using Engineered Nanofiber Substrates. PhD Thesis, National University of Singapore 2010.
Open Access
-
Niu X, Liu Z, Tian F, Chen S, Lei L, Jiang T, Feng Q, Fan Y. Sustained delivery of calcium and orthophosphate ions from amorphous calcium phosphate and poly(L-lactic acid)-based electrospinning nanofibrous scaffold. Scientific Reports 2017; 7: 45655.
Open Access
-
Schneider O D, Weber F, Brunner T J, Loher S, Ehrbar M, Schmidlin P R, Stark W J. In vivo and in vitro evaluation of flexible, cottonwool-like nanocomposites as bone substitute material for complex defects. Acta Biomater 2009; 5: 1775.
-
Schneider O D, Mohn D, Fuhrer R, Klein K, Kampf, Nuss K M R, Sidler M, Zlinszky, von Rechenberg B, Stark W J. Biocompatibility and Bone Formation of Flexible, Cotton Wool-like PLGA/Calcium Phosphate Nanocomposites in Sheep. The Open Orthopaedic Journal 2011; 5: 63.
Open Access
-
Schofer MD, Roessler PP, Schaefer J, Theisen C, Schlimme S, Heverhagen J T, Voeljer M, Dersch R, Agarwal S, Fuchs-Winkelmann S, Paletta JRJ. Electrospun PLLA Nanofiber Scaffolds and Their Use in Combination with BMP-2 for Reconstruction of Bone Defects. PLoS ONE 2011: 6(9); e25462. doi:10.1371/journal.pone.0025462.
Open Access
Schuttler K F, Bauhofer M W, Ketter V, Giese K, Eschbach D A, Yenigun M, Fuchs-Winkelmann S, Paletta J R J. Direct incorporation of mesenchymal stem cells into a Nanofiber scaffold - in vitro and in vivo analysis. Sci Rep 2020; 10: 9557.
Open Access
-
Shin M, Yoshimoto H, Vacanti J P. In Vivo Bone Tissue Engineering Using Mesenchymal Stem Cells on a Novel Electrospun Nanofibrous Scaffold. Tissue Engineering 2004; 10: 33.
-
Son S R, Linh N T B, Yang H M, Lee B T. In vitro and in vivo evaluation of electrospun PCL/PMMA fibrous scaffolds for bone regeneration. Sci Technol Adv Mat 2014; 14: 015009.
Open Access
-
Steigman S A, Ahmed A, Shanti R M, Tuan R S, Valim C, Fauza D O. Sternal repair with bone grafts engineered from amniotic mesenchymal stem cells. Journal of Pediatric Surgery 2009; 44: 1120.
-
Yun J W, Heo S Y, Lee M H, Lee H B. Evaluation of a poly(lactic-acid) scaffold filled with poly(lactide-co-glycolide)/hydroxyapatite nanofibres for reconstruction of a segmental bone defect in a canine model. Veterinarni Medicina 2019; 64: 531.
Open Access
▲ Close list
 ElectrospinTech
ElectrospinTech